CMS Releases CY 2025 OPPS and ASC Proposed Rule
The Centers for Medicare & Medicaid Services (CMS) has released the calendar year (CY) 2025 Hospital Outpatient Prospective Payment System (OPPS) and Ambulatory Surgical Center (ASC) Payment System Proposed Rule (CMS-1809-P), which includes proposals to update payment rates, policies and regulations affecting Medicare services furnished in hospital outpatient and ASC settings beginning in CY 2025.
The Proposed Rule, released on July 10, 2024, includes policies that aim to address health disparities, expand access to behavioral healthcare services and improve transparency in the health system, objectives that have been prioritized in prior OPPS rulemaking. CMS also issued requests for information (RFIs) on a number of topics, including the operating costs of tribally operated outpatient clinics, to address the appropriateness of Indian Health Service (IHS) all-inclusive rate (AIR) payments, add-on payments for high-cost treatments at IHS sites and updating the Hospital Quality Star Ratings methodology.
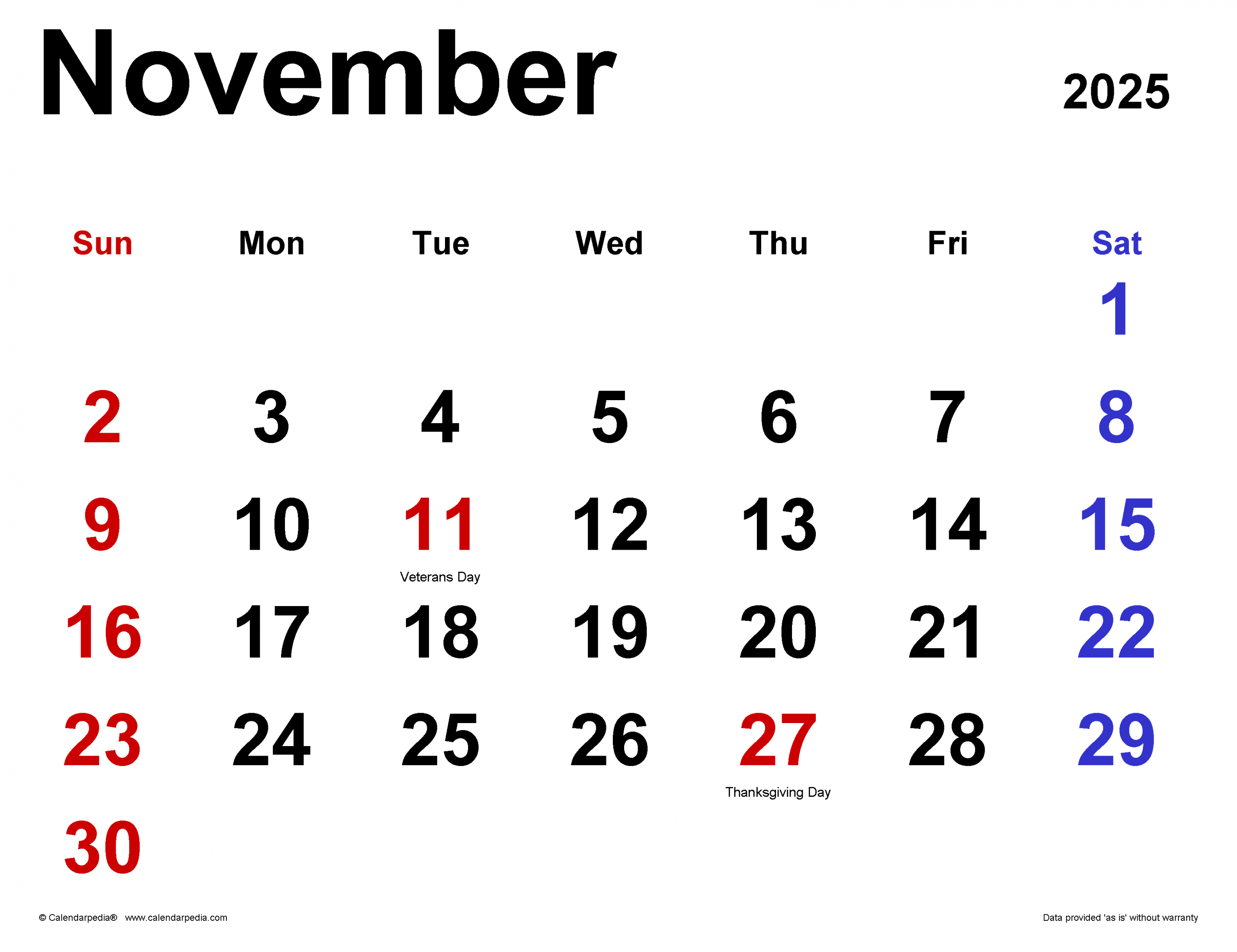
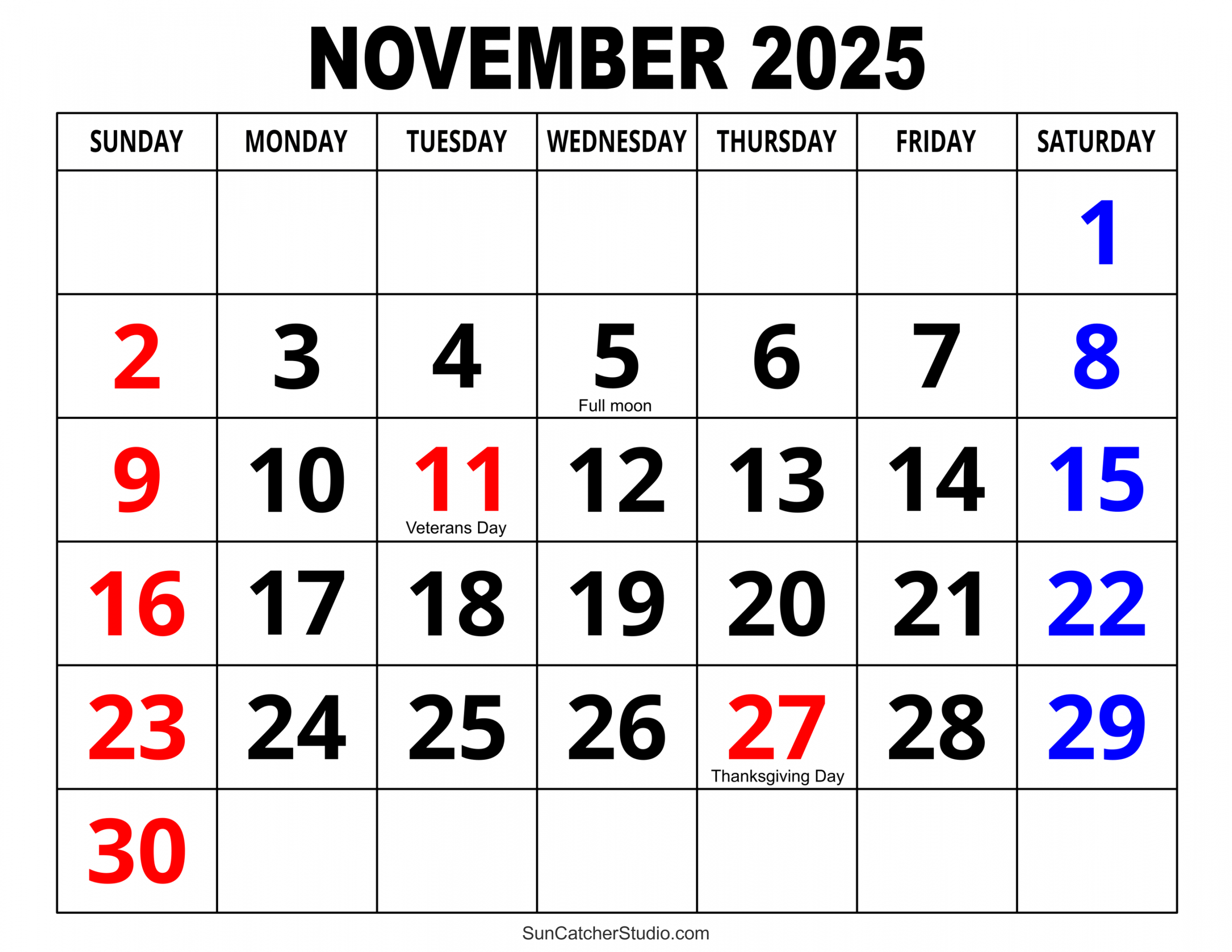
The Proposed Rule is open for a 60-day comment period that will close on Sept. 9, 2024. The Final Rule with comment is expected to be issued on or by Nov. 1, 2024.
To learn more about the OPPS and ASC Proposed Rule, review the following resources:
To access specific content in this Holland & Knight alert, use the following links:

Key Proposals of Note CMS proposes to address the maternal health crisis through new obstetrical services-specific conditions of participation. CMS proposes not to expand the categories of services subject to prior authorization, but to harmonize the timeline for review for nonurgent services and procedures. CMS introduces new quality measures focused on health equity and social drivers of health and seeks input on further addressing patient safety. CMS proposes revising its current bundling policy for diagnostic radiopharmaceuticals to pay for high-cost radiopharmaceuticals separately with a per-day cost over a specific threshold. CMS proposes revising incarceration definitions to allow for Medicare payment for services furnished to individuals on parole, probation or home detention. CMS proposes changing payment policy for investigational device exemption studies and coverage with evidence development clinical trials. CMS proposes expanding coverage of colorectal cancer screening tests. CMS proposes implementing mandatory continuous eligibility for children in Medicaid and Medicaid and Children’s Health Insurance (CHIP). CMS proposes adding exceptions to the Medicaid clinic services “four walls” requirement. CMS proposes providing add-on payment for high-cost drugs provided by IHS and tribal facilities. CMS proposes excluding qualifying cell and gene therapies from comprehensive ambulatory payment classification (C-APC) packaging and seeks comments on other potential changes to the C-APC packaging policy for future years. OPPS and ASC Payment System Updates For hospitals that meet the quality reporting requirements, CMS proposes updating OPPS and ASC payment rates by 2.6 percent for 2025, reflecting a 3.0 percent projected hospital market basket percentage increase, reduced by 0.4 percent for the productivity adjustment. This increase is 0.5 percent lower than the 3.1 percent increase implemented in the CY 2024 Final Rule. CMS aligned the fee schedule factor increase with the market basket increase factor proposed in the fiscal year 2025 Inpatient Prospective Payment System and Long-Term Care Hospital Prospective Payment System Proposed Rule. ASC Payment Update For CY 2025, CMS is proposing to adjust its ASC conversion factor to $89.379 for ASCs meeting quality reporting requirements and a conversion factor of $87.636 for ASCs failing to meet those requirements. Hospitals failing to meet the Hospital Outpatient Quality Reporting (OQR) Program reporting requirements will face an additional 2 percent reduction from the increase factor adjustment to the conversion factor used to calculate the OPPS payment rate. Ambulatory Payment Classification Group Policies New CPT Code Assignment CMS proposes assigning one current procedural terminology (CPT) code (subretinal injection of a pharmacological agent, including vitrectomy and one or more retinotomies) to ambulatory payment classification (APC) 1563 for CY 2025, as sufficient claims data is now available to determine the mean cost of administering the procedure. Solicitation of Comments HCPCS Codes: CMS solicits comments on 73 new healthcare common procedure coding system (HCPCS) codes effective April 1, 2024, and 127 new HCPCS codes effective July 1, 2024. CMS will also solicit comments on HCPCS codes effective Oct. 1, 2024, and Jan. 1, 2025, in the Final Rule. Low Volume APC Policy Universal Low Volume APC Policy: CMS proposes to retain the policy where services with fewer than 10 claims over a four-year lookback period are exempt from the New Technology APC to which they are assigned. Exemptions and Exclusions 2 Times Rule: CMS proposes exempting 23 APCs from the 2 Times Rule, which ensures that the costs of items and services within an APC group have comparable resource use. Qualifying Cell and Gene Therapies: CMS proposes excluding nine qualifying cell and gene therapies from C-APC packaging for one year, as they are considered independent therapies. CMS seeks comments on whether this proposed policy captures all relevant products. Areas for Comment on APCs Additional Exclusions: Are there other cell and gene therapies that should be excluded from C-APC packaging for CY 2025? Policy Duration and Scope: Should this exclusion proposal be extended beyond one year or should a different, expanded or supplemental policy be considered in future rulemaking? Applicability: Is it appropriate for other classes of drugs, biologicals or medical devices to be excluded from packaging with all C-APCs or only specific C-APCs, such as the Comprehensive Observation Services C-APC (Status Indicator = “J”)? New C-APC Structure: How could CMS structure a new C-APC or similar packaged payment policy for the administration of cell or gene therapies? For example, should a chimeric antigen receptor (CAR) T-cell therapy administration C-APC be created, where the CAR-T or gene therapy is integral, ancillary, supportive, dependent or adjunctive to the primary C-APC service? Associated Items and Services: What integral, ancillary, supportive, dependent or adjunctive items and services are routinely provided as part of the administration of cell and gene therapies or in conjunction with these therapies? Future Policy Revisions: Are policy revisions to the C-APC policy appropriate in future rulemaking, such as a modified outlier payment policy specific to C-APCs to address related situations in the future? Specific APC Placements Lung Cancer Screening: CMS proposes placing CPT code 71271 (low dose computed tomography (LDCT) for lung cancer screening) in APC 5522 with a payment rate of $106.30, and G0296 (visit to determine lung LDCT eligibility) in APC 5822 with a payment rate of $90.09. Drugs, Biologicals, Radiopharmaceuticals and Medical Devices Products With Pass-Through Status Continuation of Pass-Through Status: CMS proposes that 57 drugs and biologicals approved between April 1, 2023, and April 1, 2024, maintain their pass-through payment status beyond Dec. 31, 2025. End of Pass-Through Status: CMS proposes ending pass-through payment status by the end of CY 2025 for 28 drugs and biologicals initially approved between April 2022 and January 2023. Products Without Pass-Through Status Packaging Threshold: CMS proposes setting the packaging threshold at $140 for determining separate payment classifications for drugs and biologicals to ensure consistent packaging determinations. Biosimilars: CMS proposes continuing to allow separate payments for biosimilars if their reference biologicals are also paid separately. Packaging Policy for Diagnostic Radiopharmaceuticals Current Policy: CMS currently packages various drugs, biologicals and radiopharmaceuticals, including diagnostic radiopharmaceuticals, based on their use in diagnostic tests or procedures. Proposed Change: To address concerns about access for safety net hospitals and underserved communities, CMS proposes to pay separately for diagnostic radiopharmaceuticals with per-day costs above $630, approximately twice the current volume-weighted average cost of diagnostic radiopharmaceuticals. This proposal aims to maintain beneficiary access without disincentivizing the use of clinically appropriate high-cost, low-utilization agents. Pricing Methodology: CMS proposes using the mean unit cost (MUC) based on hospital claims data instead of the average sales price (ASP) methodology due to insufficient ASP reporting by manufacturers. CMS seeks feedback, however, on using ASP for future payment determinations. Add-On Payment for Select Radiopharmaceuticals Technetium-99m (Tc-99m): Since CY 2013, CMS has provided an additional $10 payment for Tc-99m produced without highly enriched uranium (HEU) to support U.S. initiatives to reduce reliance on foreign reactors and promote the production of medical radioisotopes from non-HEU sources. CY 2025 will be the final year for this add-on payment, pending certification by the Secretaries of the U.S. Department of Energy (DOE) and U.S. Department of Health and Human Services (HHS) that a sufficient global supply of non-HEU Tc-99m exists for U.S. patient needs. New Proposal: Due to concerns about the domestic supply chain for molybdenum-99 (Mo-99), the precursor to Tc-99m, CMS proposes a new $10 add-on payment per dose, beginning Jan. 1, 2026, for radiopharmaceuticals using Tc-99m derived from domestically produced Mo-99. This initiative aims to ensure equitable reimbursement for providers, reflecting the higher costs of domestically sourced products, and safeguard continued beneficiary access to essential medical resources. Payment for Devices Pass-Through Device Applications: CMS received 14 complete pass-through device applications by the March 1, 2024 quarterly deadline. Of these, 10 had received Breakthrough Device designation and U.S. Food and Drug Administration (FDA) marketing authorization, making them eligible to apply under the alternative pathway. Reassignment of Procedures: CMS proposes to continue a policy finalized in CY 2024, which reassigned four procedures (CPT codes 0308T, 0616T, 0617T and 0618T) from Level 5 Intraocular APC to a new Level 6 Intraocular APC to improve payment stability for an APC code category with a low volume of claims submitted per year. CMS, however, also proposes to replace CPT code 0616T with the new CPT placeholder code 6X004 and to delete CPT codes 0617T and 0618T. New HCPCS Codes: Due to the lack of claims data for newer HCPCS codes, CMS proposes applying the greater of 31 percent of the HCPCS code’s payment or the APC-wide device offset percentage for new procedure HCPCS codes that include the implantation or insertion of a device. New Conditions of Participation Obstetrical Services Specific Conditions of Participation
CMS has highlighted the current maternal health crisis in the U.S., which has resulted in one of the highest maternal mortality rates among high-income countries with disproportionate impact on racial and ethnic minorities. In response, CMS has undertaken various initiatives to improve maternal healthcare. In May 2024, CMS published an RFI on Obstetrical Services Standards for hospitals, critical access hospitals and rural emergency hospitals in the FY 2024 Hospital IPPS Proposed Rule, seeking public comments on developing targeted baseline health and safety standards for obstetrical (OB) services.
After examining the high rates of maternal mortality and morbidity in the U.S., reviewing feedback from stakeholders and evaluating available resources and current requirements, CMS has determined that new requirements for OB services are necessary to protect the health and safety of pregnant, birthing and postpartum patients. Consequently, CMS is proposing new Conditions of Participation (CoP) for OB services, including requirements for the organization, staffing and delivery of OB services, as well as staff training.
The proposed OB services CoPs would not reference any specific organization’s guidelines but would require that all standards set by affected hospitals be based on evidence from nationally recognized sources. The proposed requirements include:
Organization and Standards: OB services must be well-organized and meet nationally recognized standards of practice for both physical and behavioral health. Integration with Other Departments: OB services must be integrated with other departments within the facility and organized appropriately to the services offered. Supervision: An individual with the necessary education and training (e.g., a registered nurse, certified nurse midwife, nurse practitioner, physician assistant or a doctor of medicine or osteopathy) must supervise OB patient care units. Practitioner Roster: The facility must maintain a roster of all OB practitioners, detailing the privileges afforded to each practitioner, ensuring these privileges match the practitioners’ competencies. Consistency with Facility Resources: OB services must be consistent with the facility’s resources and needs. Labor and Delivery Room Suites: Labor and delivery room suites must have a call-in system, cardiac monitor and fetal Doppler or monitor. Protocols for Health and Safety Events: Facilities must have protocols for handling patient health and safety events, such as obstetrical emergencies, complications, and immediate post-delivery care. New Standard within Emergency Services CoP
To improve care for all patients, including pregnant, birthing, and postpartum women receiving emergency services, CMS proposes a new standard, “Emergency Services Readiness,” within the Emergency Services CoPs. This standard would require facilities to have protocols and provisions consistent with nationally recognized and evidence-based guidelines to meet the emergency needs of patients, and to train staff these protocols and provisions annually.
Hospitals provisions would be required to include the following:
Drugs, Blood and Biologicals: Hospitals must have drugs, blood, blood products and biologicals commonly used in life-saving procedures. Equipment and Supplies: Hospitals must have equipment and supplies commonly used in life-saving procedures. Call-In System: Hospitals must have a call-in system for each patient in each emergency services treatment area.
Hospitals would be given flexibility in identifying the provisions that would meet the needs of their patient population.
Quality and Health Equity Measures Overall Hospital Quality Star Rating Modification
To prioritize patient safety, CMS is seeking public comment on three options for updating the overall hospital quality star rating methodology and whether hospitals that performed in the bottom quartile in the Safety of Care measure group should be eligible to receive five-star ratings. The options are 1) reweighting the Safety of Care measure group, 2) reducing the rating of any hospital in the lowest quartile for Safety of Care by one star or 3) combining a weight change with a policy-based four-star maximum for any hospital in the lowest quartile.
CMS Proposes the Adoption of Health Equity Measures Across Quality Programs
CMS proposes to adopt three measures for the Hospital OQR, Ambulatory Surgical Center Quality Reporting (ASCQR) and Rural Emergency Hospital Quality Reporting (REHQR) programs, aligned with CMS’ goal of advancing health equity:
Hospital Commitment to Health Equity (HCHE) measure for the Hospital OQR and REHQR Programs and Facility Commitment to Health Equity (FCHE) measure for the ASCQR Program, beginning with the CY 2025 reporting period and impacting the CY 2027 payment/program determination. This measure uses five attestation-based domains. Screening for Social Drivers of Health measure, with voluntary reporting beginning with CY 2025 and mandatory reporting beginning with CY 2026, impacting the CY 2028 payment/program determination. The measure assesses the total number of patients screened for five specific health-related social needs (HRSNs). Screen Positive Rate for Social Determinants of Healthcare measure, with voluntary reporting beginning with CY 2025 and mandatory reporting beginning with CY 2026 and impacting the CY 2028 payment/program determination. The measure examines the number of beneficiaries who screened positive for each of the five specific social risk factors used in the screening for social determinants of healthcare measure.
Adoption of these measures is intended to align measures across CMS’ quality programs and incentivize quality reporting entities to identify and address health equity gaps.
Proposed Changes to Hospital OQR Program Quality Measures and Program
CMS proposes the following changes to the Hospital OQR measures, in addition to the health equity measures outlined above:
Adoption of the Patient Understanding of Key Information Related to Recovery After a Facility-Based Outpatient Procedure or Surgery, Patient Reported Outcome-Based Performance measure, with voluntary reporting beginning with CY 2025 and mandatory reporting beginning with CY 2026 and impacting the CY 2028 payment determination. The goal of this measure is to provide insight into the communication of recovery information and improve patient understanding of this information. Removal of the MRI Lumbar Spine for Low Back Pain measure beginning with the CY 2025 reporting period and impacting the CY 2027 payment determination, as recent studies have shown that performance on this measure did not improve patient outcomes. Removal of the Cardiac Imaging for Preoperative Risk Assessment for Non-Cardiac, Low-Risk Surgery measure beginning with the CY 2025 reporting period and impacting the CY 2027 payment determination, due to a lack of meaningful data.
CMS also proposes to modify the Hospital OQR Program’s immediate measure removal policy to an immediate suspension policy, which is used when continued use of a measure raises patient safety concerns. If an immediate suspension occurs, CMS will address the suspension and propose to retain, modify or remove the measure in the next reasonable rulemaking opportunity. This change aligns measure suspension policies across the REHQR, Hospital OQRP and ASCQR programs and is intended to increase transparency and provide opportunity for public input before a measure is potentially removed.
Additionally, CMS proposes to require that electronic health record (EHR) technology be certified to all available electronic clinical quality measures (eCQMs) to ensure hospitals can accurately capture and report the data needed for these measures.
CMS also proposes to publicly post the Median Time from Emergency Department (ED) Arrival to ED Departure for Discharged ED Patients measure – Psychiatric/Mental Health Patients strata on Care Compare. While this data is already available on data.medicare.gov, CMS believes that displaying this information on Care Compare will be useful to patients when choosing care locations, as well as for researchers and hospital staff aiming to address health disparities and improve timely access to care.
Revisions to Incarceration Definitions
Current definitions in the Medicare payment exclusion rule and eligibility requirements for the special enrollment period (SEP) for formerly incarcerated individuals create potential barriers to healthcare access for individuals returning to the community following incarceration. To remove these barriers, CMS proposes to modify the definition of “custody” within the payment exclusion rule and the eligibility requirements for the SEP.
CMS Proposes New Definition of “Custody”
Section 1862(a)(2) of the Social Security Act prohibits Medicare from paying for items or services for individuals who have no obligation to pay for those items or services. This “no legal obligation to pay” payment exclusion means that Medicare cannot cover items or services for individuals in the custody of penal authorities, as these individuals are assumed to have no legal obligation to pay for their care.
Current Definition of Custody
The current definition of “custody” at Section 411.4(b) includes individuals:
under supervised release on medical furlough required to live under home detention confined completely or partially in any way under a penal statute or rule
This definition effectively prohibits Medicare from paying for services for individuals on parole, probation, bail or supervised release.
Proposed Changes to the Definition
To increase access to care for individuals returning to the community following incarceration, CMS proposes to amend the definition of “custody” at Section 411.4(b) by removing:
“under supervised release” “required to live under home detention” “confined completely or partially in any way under a penal statute or rule”
Additionally, the proposal clarifies that individuals “required to reside in mental health facilities” only includes those required to reside in such facilities under a penal statute or rule. These changes would allow Medicare to cover healthcare for individuals on parole, probation or home detention.
Request for Comments
CMS seeks comments on:
examples where these individuals already have a legal obligation to pay for their healthcare situations where these individuals receive services typically furnished by government agencies at no cost how these policies should apply to individuals required to reside in halfway houses Other Notable Proposals Remote Services (Diabetes, Medical Nutrition, Mental Health)
CMS notes that the agency recognizes that for the past several years, through the public health emergency (PHE) for COVID-19 and several legislative extensions of PHE-related flexibilities for Medicare telehealth services, the agency has “generally aligned” payment policies for outpatient therapy services, diabetes self-management training (DSMT) and medical nutrition therapy (MNT) services furnished remotely by hospital staff to beneficiaries in their homes with policies for Medicare telehealth services. CMS states that “to the extent that therapists and DSMT and MNT practitioners continue to be distant site practitioners for purposes of Medicare telehealth services, CMS anticipates aligning the agency’s policy for these services with policies under the Physician Fee Schedule (PFS) and continuing to make payment to hospitals for these services when furnished by hospital staff.
Inpatient Only List
CMS proposes to add three services to the inpatient-only list, which includes services that should only be performed inpatient due to their complexity and the level of post-operative care required (CPT codes 0894T, 0895T and 0896T).
Partial Hospitalization Services
CMS proposes updates to the payment rates for Partial Hospitalization Programs (PHPs) and Intensive Outpatient Programs (IOPs) furnished in HOPDs and Community Mental Health Centers (CMHCs). The Proposed Rule includes revisions to the coding and billing requirements for PHP and IOP services to support accurate reimbursement and better alignment with the actual services provided. The proposed payment rates for CY 2025 are based on CY 2023 claims data and available cost information. CMS proposes an outlier policy for CMHCs to provide additional payments for high-cost cases in PHP and IOP services.
Review Timeframes for the HOPD Prior Authorization Process
In CY 2020, CMS established a nationwide prior authorization process and requirements for certain outpatient department (OPD) services. Providers must submit a prior authorization request to the Medicare Administrative Contractor (MAC) for services included on the list of OPD services that require prior authorization. These services currently include:
blepharoplasty rhinoplasty botulinum toxin injections panniculectomy vein ablation cervical fusion with disc removal implanted spinal neurostimulators facet joint interventions
In the CMS Interoperability and Prior Authorization Final Rule, CMS finalized for Medicare Advantage and other plans that response times of seven calendar days for standard prior authorization requests. Even though Medicare wasn’t subject to this rule, CMS proposes to align the timeframe for prior authorization requests for fee-for-service hospital outpatient services to seven calendar days, instead of 10 business days, for standard reviews.
CMS states that this change would not only streamline the prior authorization processes so that they are the same across payers but would also help to reduce provider burden by having the same timeframe and reducing the potential for delays in care by decreasing the time beneficiaries and providers wait for prior authorization decisions on standard requests in fee-for-service Medicare.
Continuous Eligibility for Children in Medicaid and CHIP
In alignment with the Consolidated Appropriations Act, 2023 and to ensure continuous eligibility (CE) in Medicaid and CHIP for children under 19, CMS proposes to make CE mandatory for all states. This change would remove previous state options to limit CE to younger age groups or shorter periods. Additionally, the Consolidated Appropriations Act, 2023 aligns CHIP’s CE policy with Medicaid, removing the option for states to disenroll children for nonpayment of premiums or enrollment fees during the continuous eligibility period. States may still collect enrollment fees before initial enrollment or re-enrollment and can disenroll children with unpaid premiums at the end of the 12-month CE period, following required grace period protocols. This alignment ensures consistent coverage protections across both Medicaid and CHIP. The current Medicaid regulation includes exceptions that allow states to terminate coverage during a continuous eligibility period if the child or representative requests it, if eligibility was erroneously granted due to agency error or fraud, or if the child is deceased. These exceptions remain unchanged to maintain program integrity.
Medicaid Clinic Services Four Walls Exceptions
Under law, states may choose to offer certain Medicaid benefits to categorically needy and medically needy Medicaid beneficiaries. Clinic services are one of these optional benefit categories. The first type of services included in the benefit are services furnished at the clinic (the “four walls” requirement) by or under the direction of a physician or dentist.
CMS is proposing three exceptions:
First, CMS proposes an exception for IHS and tribal clinics, allowing them to provide services outside the clinic walls. This change would be mandatory for all states that opt to cover Medicaid clinic services. Second, CMS proposes creating an optional exception for clinics primarily organized to treat outpatients with behavioral health disorders, including mental health and substance use disorders. These clinics would be allowed to provide services outside the clinic walls, including nonbehavioral health services. This exception is optional for states. Third, CMS proposes an optional exception for clinics located in rural areas (excluding rural health clinics), allowing them to offer services outside the clinic walls. This change aims to improve access to healthcare services for residents in rural areas who often lack access due to distance and transportation challenges. States can choose to adopt this exception to better serve their rural populations.
These exceptions are designed to remove barriers to accessing care for vulnerable populations, ensuring they receive necessary services regardless of their ability to visit a clinic in person.
Blended Payment Policy for IDE Studies and CED Clinical Trials
In the CY 2023 OPPS/ASC Final Rule, CMS established a policy to make a single blended payment for devices and services in Category B investigational device exemption (IDE) studies to preserve the scientific validity of these studies. This policy involves creating or revising HCPCS codes to describe Category B IDE studies, including both treatment and control arms, along with routine care items and services. The single blended payment rate takes into account the frequency of device use compared to the control group, averaging the payment for the device with zero payment for the control in a 1:1 ratio. CMS has clarified that this policy only applies to IDE studies with a control arm; studies without a control arm are paid using standard Medicare payment methodologies.
For CY 2025, CMS is proposing technical refinements to Category B clinical trials coding and payment policy for devices and procedures. CMS is also proposing to extend coding and payment policy to drugs and devices that meet the Medicare Coverage and Analysis Group’s coverage and evidence development (CED) requirement for which there is a control arm. CMS clarified that Category B IDE studies with no control arm are payable under normal methodology versus not payable. CMS proposes a similar policy for payment of devices under a CED national coverage determination (NCD) – e.g., a single blended payment rate that would be dependent on the specific trial protocol.
CMS proposes payment of drugs at an adjusted payment level representing the frequency with which the study drug and placebo (or comparator) is furnished. The base payment amount for the study drug is proposed to be ASP + 6 percent. If no ASP data is available, then CMS proposes to pay wholesale acquisition cost (WAC) with initial sales period at WAC + 3 percent otherwise at WAC + 6 percent. If no WAC data is available, CMS proposes to pay 95 percent average wholesale price. The placebo/comparator would be assigned “zero dollar” and used with the drug amount to determine a blended rate.
The proposed policy aims to preserve the scientific integrity of clinical trials by preventing differences in Medicare payment methods from revealing patient group assignments. CMS will cover routine costs for approved clinical trials, with payment adjustments established only when necessary to prevent unblinding the trial.
CMS seeks comments on potential scenarios where Medicare payment methodologies might interfere with the scientific validity of a trial.
Coverage Changes for Colorectal Cancer (CRC) Screening Services
For CY 2025, based on public input and consultation with specialty societies, and as discussed in the CY 2025 PFS Proposed Rule, CMS proposes to update and expand coverage for CRC screening.
As discussed in the CY 2025 PFS Proposed Rule, CMS proposes to make the following revisions:
remove coverage for the barium enema procedure add coverage for the computed tomography colonography (CTC) procedure expand the existing definition of a “complete colorectal cancer screening” to include a follow-on screening colonoscopy after a Medicare-covered blood-based biomarker CRC screening test AIR Add-On Payment for High-Cost Drugs Provided by the IHS and Tribal Facilities
CMS states that in light of the equity and beneficiary access concerns that prompted the agency’s CY 2024 comment solicitation and the input received in response to that solicitation, the agency proposes, starting Jan. 1, 2025, to separately pay IHS and tribal hospitals for high-cost drugs furnished in hospital outpatient departments through an add-on payment in addition to the AIR using the authority under which the annual AIR is calculated.
CMS is seeking comment on how to best apply an add-on payment model, calculation and proposed implementation plan. CMS issued an RFI regarding the relative operating costs of tribally operated outpatient clinics, as well as feedback and supporting evidence to address whether or why payment set at the IHS AIR would be more appropriate than payment rates under the federally qualified health center PPS.
RFI on Paying All IHS and Tribally Operated Clinics the IHS Medicare Outpatient AIR
CMS is seeking information on several aspects of these proposals, including the kinds of and number of facilities or clinics that the Medicare outpatient IHS AIR could apply to; that is, it is unclear whether the Tribal Technical Advisory Group anticipates that these facilities enroll in Medicare as FQHCs going forward, or whether they are referring to FQHCs that are currently paid under the FQHC PPS.